This week on the blog we are highlighting an oral presentation given at this year’s annual American Anthropological Association conference in Washington D.C. by Jonathan Metzl entitled Negroes With Guns: Mental Illness, Gun Violence, and the Racial Politics of Firearms. The session was named “Critical Inquiries: Violence, Trauma, and the Right to Health” on Thursday, November 30, 2017. Metzl combined historiographical and ethnographic analysis to explore the connections between gun violence, mental illness, and shifting anxieties about race in the United States. Metzl discussed how decisions about which crimes American culture diagnoses as “crazy,” and which crimes it deems as “sane,” are driven as much by the politics and anxieties of particular cultural moments as by the innate neurobiologies of particular assailants. The presentation concluded by describing how racialized questions of whether “the insane” should be allowed to bear arms become the only publicly permissible way to talk about questions of gun control while other narratives, such as the mass psychology of needing so many guns in the first place or the anxieties created by being surrounded by them, remain silenced.

Metzl began his presentation by stating that after the recent and tragic Las Vegas mass shooting, he gave 58 interviews in only two days on “the insane politics of mass shootings.” The two main questions that get asked after each mass shooting are: “Is mental illness the cause of mass shootings?” and, “Will treating mental illness stop gun crime?” Both conservative and liberal media analyses include these types of questions, whether or not they ultimately claim mental illness as the answer (for example: NPR’s On Point, Politico, and Fox News).
Yet Metzl asked, why do these mental illness questions follow after mass shootings? “Aren’t these questions starting to be ridiculous?” Metzl asked, after referring to a study published in the journal Aggression and Violent Behavior which found some mass murderers and serial killers have something in common: autism and head injury. Yet this study was criticized for fueling judgments about an entire section of society and further contributing to the mental illness-gun violence debate.
 In some ways, linking mass shootings and mental illness makes sense. Mass shootings are beyond the realm of “sanity” and understanding. Metzl stated that constructing a binary of sane vs. insane, good vs. evil, may be a means of processing grief and uncertainty. Further, many of the mass shooting perpetrators in the last decades have displayed some kind of mental illness symptomatology before their crimes. Mother Jones published an investigation of US mass shootings from 1982-2017 including information on the shooter’s race, gender, prior signs of mental health issues, mental health details, and whether or not the weapons were obtained legally. But this information cannot lead to a causal argument.
In some ways, linking mass shootings and mental illness makes sense. Mass shootings are beyond the realm of “sanity” and understanding. Metzl stated that constructing a binary of sane vs. insane, good vs. evil, may be a means of processing grief and uncertainty. Further, many of the mass shooting perpetrators in the last decades have displayed some kind of mental illness symptomatology before their crimes. Mother Jones published an investigation of US mass shootings from 1982-2017 including information on the shooter’s race, gender, prior signs of mental health issues, mental health details, and whether or not the weapons were obtained legally. But this information cannot lead to a causal argument.
These types of questions have ideological and political roots, and focusing exclusively on issues of mental health force other concerns out of the debate. At a National Rifle Association (NRA) press conference in December 2012, chief executive Wayne LaPierre suggested having “an active national database for the mentally ill” would help prevent gun violence. In 2013, Ann Coulter wrote a Sound Off on Fox Nation entitled “Guns Don’t Kill People, The Mentally Ill Do.” After the 2015 Planned Parenthood shooting in Colorado Springs, Paul Ryan called for a need to look at fixing our nation’s mental illness health system, not it’s gun legislation. Most recently, following news of the mass shooting of parishioners at a Sunday service at a small Baptist church in Texas, Trump proclaimed mental health was the overarching issue, not gun control, even before complete details of the shooter were known.
Following this overview of political ideologies shaping the mental illness conversation, Metzl then asks, “What can reasonably minded people do to push back?”
Metzl then presented five talking points about important ways to push back against the mental-illness-and-mass-shooting account while still remaining respectful of mental illness, treatments, and medications. These talking points discuss why this association is problematic.
1. “It’s sample bias – and dangerously so…”: Mass shootings come to stand for all shootings. But mass shootings are not the only time we need to talk about gun violence, Metzl stated. When we talk about mass shootings, we are not talking about policy implications for everyday gun death. Every day gun violence, gun proliferation, the ability to buy guns through loop holes should all be part of the national conversation. Worryingly, Metzl states, the situation is about to get much worse. Today (Wednesday, December 6, 2017) the House will vote on a “concealed carry reciprocity” bill, creating a national blanket right to carry a concealed weapon across state lines. For Metzl, the point overall is that the mental illness narrative distracts from daily gun violence and the political negotiations behind gun regulations.
2. “It’s stigmatizing and misrepresentative…”: Fewer crimes involve people with mental illness. People with sanity are much more dangerous, Metzl stated. People diagnosed with a mental illness are less likely to shot other people, therefore we should really be restricting guns from the sane. Further, Metzl stated that statistically there is no predictive value in using a mental illness diagnosis for gun crime. Individuals with mental illness are more likely to be shot by police than to do the shooting themselves.
3. “It constructs false psychiatric expertise…”: Psychiatrists are being told they should be able to predict which of their patients may commit violent act. Yet the pool of people they see are not a high risk population. Metzl stated the public culture of fear may lead psychiatrists to feel culpable for the actions of their patients, over-report their concerns, and complicates the doctor-patient confidentiality bond. In the weeks before the Aurora, Colorado movie theater shooting, shooter James Holmes was seeing a psychiatrist specializing in schizophrenia. In June 2012 The Brian Lehrer Show discussed how psychiatrists determine red flags with their patients and when behavior is concerning enough to warrant further action with Columbia University Director of Law, Ethics, and Psychiatry Paul Appelbaum.
4. “It detracts from awareness of true predictive factors for everyday gun violence…”: The mental illness narrative also detracts from other risk factors for everyday gun violence and mass shootings. Substance use or abuse, past history of violence, lack of gun training, social networks, and access to firearms are all important predictive factors for gun violence.
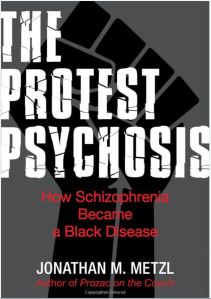 5. “It’s racist…”: Last but certainly not least, the construction of a mentally ill, dangerous, white, male, gun-owning “loner” is a political choice. The intentional presentation of the individual-isolated-from-society is not supposed to be representative of white culture. Yet in the 1960s, the FBI openly blamed “crazy” black “culture” for the rise of public black activist groups. In debates leading up to the Gun Control Act of 1968, the U.S. Government and mainstream US culture proclaimed links between African American political protest, guns, and mental illness in ways that intensified fears about black activist groups. For example, FBI profilers diagnosed Malcolm X with “pre-psychotic paranoid schizophrenia” and with membership in the “Muslim Cult of Islam” while highlighting his militancy and his “plots” to overthrow the government. The FBI also hung “Armed and Dangerous” posters throughout the southern states warning citizens about Robert Williams, the controversial head of the Monroe, North Carolina chapter of the NAACP author of a manifesto, Negroes With Guns, that advocated gun rights for African Americans. According to the posters, “Williams allegedly has possession of a large quantity of firearms, including a .45 caliber pistol… He has previously been diagnosed as schizophrenic and has advocated and threatened violence.”
5. “It’s racist…”: Last but certainly not least, the construction of a mentally ill, dangerous, white, male, gun-owning “loner” is a political choice. The intentional presentation of the individual-isolated-from-society is not supposed to be representative of white culture. Yet in the 1960s, the FBI openly blamed “crazy” black “culture” for the rise of public black activist groups. In debates leading up to the Gun Control Act of 1968, the U.S. Government and mainstream US culture proclaimed links between African American political protest, guns, and mental illness in ways that intensified fears about black activist groups. For example, FBI profilers diagnosed Malcolm X with “pre-psychotic paranoid schizophrenia” and with membership in the “Muslim Cult of Islam” while highlighting his militancy and his “plots” to overthrow the government. The FBI also hung “Armed and Dangerous” posters throughout the southern states warning citizens about Robert Williams, the controversial head of the Monroe, North Carolina chapter of the NAACP author of a manifesto, Negroes With Guns, that advocated gun rights for African Americans. According to the posters, “Williams allegedly has possession of a large quantity of firearms, including a .45 caliber pistol… He has previously been diagnosed as schizophrenic and has advocated and threatened violence.”
These historical narratives were linked to black culture, not black individuals. Issues of race and insanity produced black male bodies coded as insane. This association fostered fears that helped mobilize significant public and political sentiment for gun control. Yet there are very different politics of the present day. Metzl states were are in a time when white shooters with mental illness beget reaffirmations of gun rights and groups that advocate anti-government platforms and support broadening of gun rights, such as the Tea Party, take seats in Congress rather than being subjected to police scrutiny. For much of our country’s history, guns marked whiteness.
Metzl concluded his presentation with a discussion of a helplessness narrative. There is a kind of inaction about calling mass shootings and gun violence part of mental illness. Since we can not do anything about whether or not individuals have mental illness, it allows us to ignore the other issues and risk factors. This further constructs a kind of persons, not a composition of something larger and more systemic. The learned helplessness surrounding gun crime in the US makes hard rhetorical work to not look at whiteness and mass culture as part of the problem.
Jonathan Metzl, MD, PhD is the Frederick B. Rentschler II Professor of Sociology and Medicine, Health, and Society, Director for the Center for Medicine, Health, and Society, and Professor of Psychiatry at Vanderbilt University. He is also the Research Director of the Safe Tennessee Project, a non-partisan, volunteer-based organization that is concerned with gun-related injuries and fatalities in the United States and in the state of Tennessee. His areas of expertise include mental illness and gun violence with a particular focus on gender and race.
Learn more about Jonathan Metzl at his website, available here.









